ACCESS TO VORASIDENIB IN THE UK
VORASIDENIB
SMC SUBMISSION
PATIENT EXPERIENCES
WATCH AND WAIT PATIENTS AND THEIR CARERS/FAMILY MEMBERS
K
“My daughter is 26, autistic and suffers immensely with waiting and then visiting hospitals and not knowing what treatment she will have in respect of her LGG. She is currently on watch and wait until Jan 2026. The idea of taking a pill rather than going through all other treatment would be life changing as currently she thinks her only options going forward will be operations and chemo or radiotherapy. More invasive treatments have already given her suicidal thoughts and she has suffered deep depression and anxiety as a result. Vorasidenib would and does give us hope she can get through this with as little mental health issues as possible”.
K
“I cannot express how much it takes it out of us every time we have a hospital appointment booked.
As a carer of an autistic person receiving any medical appointments we must plan and organise so far in advance due to my daughter’s massive anxiety. We must think about the language we use, the level detail we go into, the meeting length. We often must have 2 of us take her as we don’t know how she will react to news. We both must take time off work to do this and often meetings at the hospital can take longer due to my daughter anxiety, meltdowns etc. it has a huge effect on our mental wellbeing too as it is very tiring and can wipe out a whole day for us whereas a person with no mental health needs can come and go to an appointment in the allotted time And probably get on with their day. We unfortunately don’t have that as it takes us time to talk events through my daughter after or give her rest time after to process things. If her mental state is not good, she sometimes has to stay with us overnight until she feels less anxious. As a result of this both my husband I and must plan our work around appointments and plan to work at home or work outside of work hours to make up for lost time. I have had to have counselling because of my daughters diagnosis to come to terms with this additional need in her life”.
VORASIDENIB PATIENTS AND THEIR CARERS/FAMILY MEMBERS
J
“As a parent of a young woman using vorasidenib it would be catastrophic for her to have this withdrawn. My daughter had anxiety and depression on diagnosis of the tumour.
After the operation to remove some of the tumour she physically recovered and through work, which is to her a meaning to live, much of the anxiety and depression reduced and with the use of vorasidenib so gained a normal quality of life uplifted by working and gaining friends, so much so she trains people in physical exercise. Removal of this drug would mean, giving up her job, and spiralling back into depression, for she would prematurely have to have radio therapy and chemotherapy. This besides losing her wages, and claiming benefits would destroy her mentally.
Vorasidenib has given my daughter a life back for as long as this drug is available to remove it would make her as a shell of a person and would have a disastrous effect on me and her”.
S
“I have a grade 2 astrocytoma. In July 2021 I underwent a craniotomy and was then placed on ‘watch and wait ‘. It was so hard to cope knowing that the tumour would likely grow/return. I was absolutely petrified every time I felt a slight odd pain or headache. I also was so fearful when my scan was due. My anxiety levels were sky high – my mental health suffered badly. In March 2024 I was told my scan showed some growth in the tumour, resulting in my mental health plummeting further and I stopped work.
In May 2024 I was lucky enough to be accepted on a named patient programme for Vorasidenib. Life is still very hard, but knowing I am actually receiving some treatment I have felt much more hopeful. My anxiety has improved as have my seizures. Given my age, 28 years, I feel I have a lot to give and a lot of living to do. I wish to try to avoid radio/chemo for as long as I possibly can – I have read a lot about the effects on the brain and utter disruption to day-to-day life. Life will never be the same for me but since my diagnosis this is the most ‘normal’ I have felt, I feel less isolated and have returned to work”.
C
“I was diagnosed with a brain tumour after several episodes of losing consciousness in October 2021. I was determined to carry on working as a fitness instructor until I fell off a high stage after teaching a spin class and hurting myself. I was forced to give up my passion and being self-employed I lost my income overnight. From then on, I had to move back in with my Dad.
I was referred to the local neurology centre in who recommended my best long-term outcome was to undergo surgery to remove as much of the tumour as possible, with it being in my motor area they couldn’t remove it all without permanent paralysis. I had surgery January 2022 waking up unable to move my right side at all. I sunk into a deep depression and did not want to live if I was paralysed. However, my surgeon gave me some hope and told me I could get most movement back if I really worked at physio. Which I did, initially learning to walk, eat and care for myself again. It took 18 months of rehab where I fought tooth and nail to get myself back to a place where I was finally able to work again in a part employed role, this made all the hard work worthwhile, as I just want to help people and help others feel better.
In 2024 I qualified as a personal trainer specialising in cancer and illness rehab. For example, one of my clients is returning to activity after partial lobectomy of a lung due to lung cancer. I also aim to push myself physically and raise awareness of brain tumours.
Unfortunately, In May this year I suffered a seizure, and a subsequent MRI showed tumour regrowth. My oncologist applied for me to go onto targeted medication Vorasidenib. Which allowed me to continue living independently, caring for my elderly parents, and working. This gave me hope and helped my passion for helping people, fundraising, and demonstrating what people with cancer and or disabilities can achieve. For example, obtained the mixed doubles world record of the deadly dozen fitness race. None of this would be possible without Vorasidenib treatment.
The only alternative treatment if Vorasidenib was not available would be for me to have radiotherapy and a year of chemotherapy. As you are well aware these are aggressive and debilitating treatments, especially when targeted onto the brain, I would likely have right sided movement loss, requiring me to be in 24 hour care, unable to look after my parents, be unable to work and having no quality of live.
J
“Having Vorasidenib has given us a huge part of our life back. Prior to my daughter receiving the drug it felt like we were living with little hope and I suffered from extreme anxiety. She was 27 when diagnosed and our world shattered.
‘Watch and Wait’ is so incredibly damaging to our mental health as a family. You live from scan to scan, you get more and more terrified as the scan approaches and sob with relief if the scan result shows no change. This is not a sustainable existence for any family and it is incredibly harmful.
With Vorasidenib, our anxiety levels reduced considerably. I felt like there was more chance of my daughter living a normal life and avoiding chemo/radio for some years and the damage such treatments can cause. While the drug is in its early days, it gave us hope. We could get back to work, we could all concentrate and focus better, which we needed to do to live our lives productively. We’ve even been able to organise her wedding which we couldn’t even dream of before the drug was prescribed.
Put simply, Vorasidenib has given us our lives back as a family to a considerable degree and given us much needed hope. We’re now all functioning, economically active family members with more stable mental health. If Vorasidenib was taken from us I fear for our future and whether we would cope at all.
My daughter’s neurosurgeon has explained to us the harm chemo/radio therapy can cause and how Vorasidenib is hopefully able to delay these treatments for an unknown (potentially indefinite) period of time.
My daughter is bright, active and works as a senior teacher at a secondary school but if she were to go through chemo/radio it is quite likely that the cognitive impairment she would sustain could end her career”.
M
“I’m a pragmatic person and appreciate death is a part of living, I will caveat that with this though, quality of life is more important than quantity.
What Vorasidenib does, for me certainly, is allow me to live a full life as much as anyone can with a looming terminal illness. I can work and crucially I can avoid the trauma, both physical and mental, of the alternative treatments and I am allowed hope.
To have to tell my daughter and those I love and am loved by that this lifeline will be cut off is the hardest part.
It’s an incredible feat these researchers have pulled off creating a drug that can cross the blood/brain barrier and it is a testament to our innovative spirit as a species. We all deserve a chance to live the best life we can, this disease is not a self inflicted condition. It’s a ticking time bomb and this drug is the safety mechanism that prevents the explosion.
A
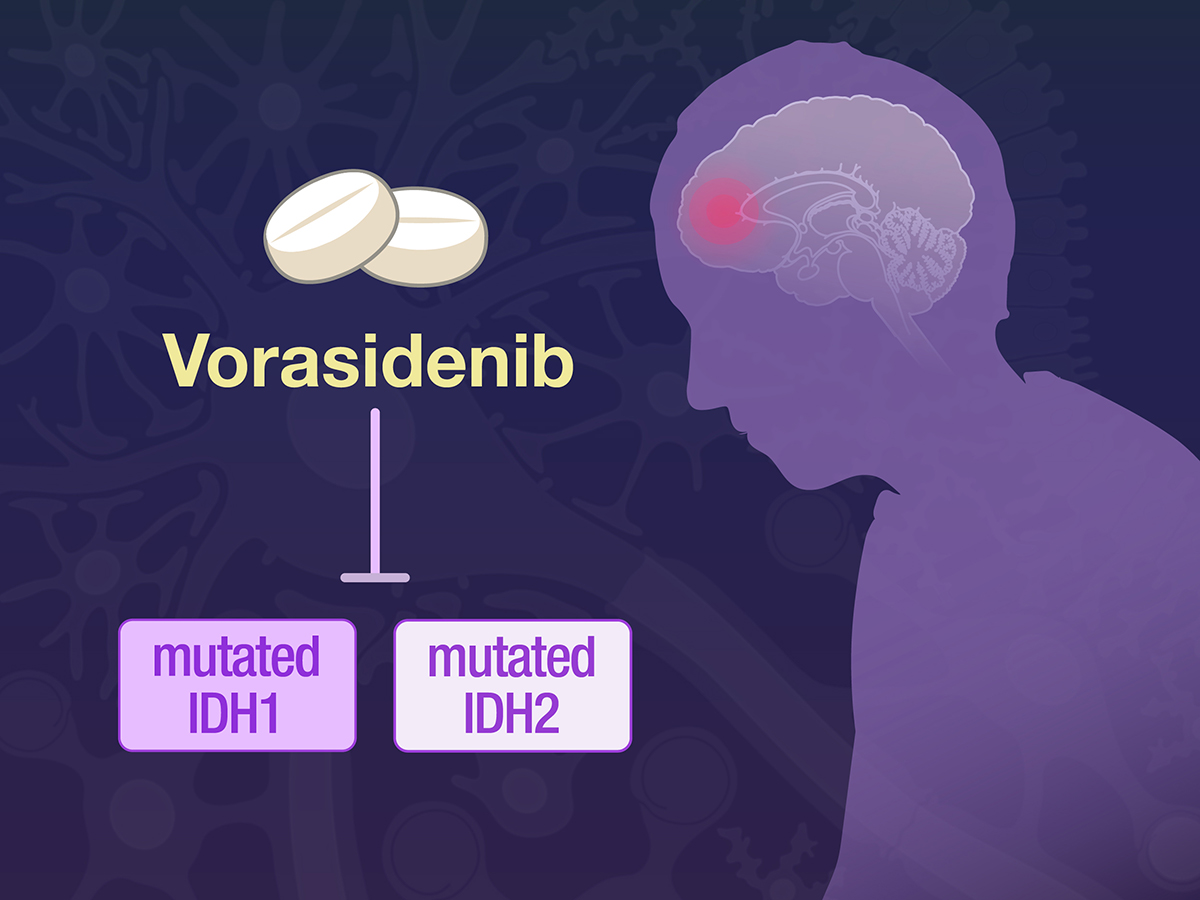
“My son had his first seizure last November and was subsequently diagnosed as having a large brain tumour. This came as a massive shock not only to him but to every family member. My son is a father, a beloved son and brother. We were told that this tumour was most likely Grade 3 with the expectation that it may have already moved towards being Grade 4 or was at the point of doing so. My son had a Craniotomy during which approximately 80% of the tumour was removed. We were all massively thankful for his successful outcome and to the wonderful team. Even more so when it was confirmed that it was still Grade 2 ,an Astrocytoma with IDH mutant gene although this could turn to a higher grade at any point.
My son recovered well and was given the opportunity to take Vorasidenib- which we were all supportive of. Chemo and Radiotherapy have very damaging long term effects on the brain meaning patients often have cognitive difficulties with motor difficulties too.
My son recovered well and has been working to support himself financially and his daughter. He still has to cope with fatigue and seizures – for which he takes medication – but Vorasidenib gives him the hope of a longer and productive life.
As a family we have seen the huge effort he puts in to keeping a healthy lifestyle to ensure that he remains alive and thriving in the face of this devastating illness. We all feel anxious and involved at every point on his journey.
Vorasidenib is the only drug to successfully cross the blood brain barrier and prove effective in halting growth for LGG brain tumour patients.
J
“Vorasidenib has given our son, and others living with Low Grade Gliomas (LGGs), hope for the future as these tumours almost always progress to become High Grade which are invariably fatal.
Our lives changed forever when our 25-year-old son was given the stomach lurching diagnosis of a brain tumour by the local hospital. The emotional pain and shock were and are indescribable. Our son’s diagnosis was devastating to him, to his partner, to us and to his sister. He was very afraid and said “Mum, am I going to die?”, no words a mother ever wants to hear. His fear filled me. The crass and callous comments of the consultant at the local hospital made our son feel even more anxious and afraid. We were left feeling crushed and helpless. There was no relief from the nightmare.
The impact on him and us was and is beyond words. I hid my anxiety from my son and would go to the bathroom to weep. I could not sleep or eat and was in no fit state to work and so took unpaid leave in order to process my son’s diagnosis and to support him. I was unable to emerge from my private grief and make proper contact with friends and other family members. There was a feeling of disbelief as you are so consumed by pain and yet the rest of the world is carrying on oblivious to your devastation. As a family we could not share one another’s feelings; there was no emotional room left over to even acknowledge them. We were all broken.
Our son withdrew. He started to train excessively and finally admitted he did this as the pain of exercise was the only time he was not thinking about the brain tumour. I wondered if his depression and anxiety and difficulty in planning and organising were all linked to the frontal lobe tumour. I sensed his feeling of fear, isolation and vulnerability.
The next few weeks were a blur of scans, tests and worry. Another admission to the local hospital brought with it bleak moments of despair.
Having been referred on to hospital our son underwent tumour resection in February 2020, and biopsy later identified the tumour as an astrocytoma. Most of the tumour was successfully removed, however we were told that the chances of tumour regrowth were “one hundred per cent”. We felt powerless and desperate. We needed hope otherwise there was only darkness.
As a parent it is like waking up in a nightmare with no way out. There is no relief from the anxiety and sadness. It is all consuming. It is the first thing you think of when you wake up, and having struggled throughout the day, the last thing you think of at night. How our son must have felt is unimaginable. There was no hope as there had been no drug treatments in the preceding 20 years. We were in a very dark place and needed hope to exist.
In 2022 an MRI scan showed evidence of tumour regrowth and our son was referred to the local neuro centre where there followed a period of ‘watchful waiting’, a state of uncertainty which was frustrating and stressful and made us feel constantly anxious. Then, in 2023, the neuro-oncologist told us that tumour had grown further and that our son’s condition had reached a stage at which there was a mandate for radiotherapy and chemotherapy. In the meantime, we had become aware of the Indigo trial and the success of Vorasidenib however, although our son was clinically eligible to participate, the trial had closed. This was obviously hugely disappointing.
By early 2024 preparations were made for our son to commence 6 weeks of daily radiotherapy followed by 18 months of chemotherapy. The negative impact on him was immense. We were all devastated. He was a highly active and competitive athlete, and the prospect of these treatments had an immediate detrimental effect on his physical, psychological and emotional wellbeing. Plans he had made would have to be cancelled and his life put on hold. Then, immediately prior to commencing radiotherapy, the hospital offered our son access to Vorasidenib on a compassionate use basis. Our son was ecstatic, as were we! His quality of life would now not be affected by arduous radiotherapy and chemotherapy treatments and its side effects, and instead of the onerous regime of daily travelling to the hospital, he could take oral medication at home. This was an immense relief. He could now carry on with his everyday life and reinstate his plans.
Our son has now been taking Vorasidenib every day since May 2024. He has been having MRI scans at three monthly intervals and thankfully the tumour has remained stable with no further regrowth. Additionally, four weekly blood tests show that he is tolerating the drug well with minimal side effects.
Vorasidenib has given our son, his partner, and his family hope, something none of us had before. For the first time we can dare to be optimistic for the future. He is able to carry on with his work and leisure activities and lead a normal life.
Vorasidenib improves quality of life and gives hope when previously there was none. By giving hope, this new drug manages to reduce anxiety for both the patient and his/her family, who previously felt powerless and desperate, living with the relentless fear of the unknown and wondering when and how fast the tumour would progress. There is now a possibility that tumour growth will be halted.
‘Watchful waiting’ results in a state of uncertainty and continuous stress just waiting for the time bomb to explode.
Radiotherapy and chemotherapy cause anxiety due to the worry of both short term and long term side effects of both, particularly a decline in cognitive function. The fear of tumour progression and undergoing existing treatments cause physical, psychosocial and emotional distress. The list is endless but includes:-
General anxiety
Scan anxiety
Insomnia
Anorexia
Low mood
Depression
Sadness
Helplessness (there is a feeling of living in a perpetual nightmare with no way out)
Despair
Isolation (as others are carrying on oblivious to your devastation)
Negative impact on work, causing financial loss and hardship
Unable to drive, causing loss of independence and, in some cases, employment
Loss of self esteem because of the above
Adverse effects on partner, children and family
When undergoing radiotherapy and chemotherapy:
Plans cancelled and life put on hold
Unable to participate in competitive sport
Unable to attend social events including weddings
Vorasidenib mitigates some of the above and enables a return to normal life. The development of Vorasidenib means there is optimism for the future for the first time”.
H
In November 2019 our son, then 25, was diagnosed with a Grade 2 Astrocytoma IDH2 brain tumour. The news was obviously devastating. In February 2020 he underwent surgery during which most of the tumour was successfully removed.
Regular MRI scans over the following two years showed no tumour regrowth, but in 2023, following a referral, regrowth began to become apparent and was confirmed as being definite in February 2024.
Our son was consequently in the process of clinical preparation for radiotherapy and chemotherapy when we received notification that the drug Vorasidenib had become available on a humanitarian, named-patient basis. This news was immensely encouraging, both for our son and for his partner and for us, his family; we had all been dreading the considerable downsides of the standard treatments. We had heard about Vorasidenib and the optimism it had generated in the USA but had hitherto been under the impression that it was unavailable in the UK. So, this was great news, and the neuro oncologist promptly changed our son’s course of treatment from radiotherapy and chemotherapy to a daily oral dose of Vorasidenib. Since then, regular scans at three monthly intervals have shown complete stability and no tumour regrowth. Monthly blood tests have shown our son to be very tolerant of the drug with minimal, if any, side effects.
We wrote earlier this year that the then four stable MRI scan results since he commenced taking Vorasidenib had given our son a growing sense of optimism for his future and he is pinning his hopes on having continued access to this excellent treatment which is, on the strong and growing evidence of our personal experience, showing signs of being effective at slowing or halting tumour progression.
Over the last 18 months, our son’s emotional state has continued to follow a cautious but upward trajectory as each three-monthly scan has delivered good news. In the last six months he and his partner have purchased their first property, and their small businesses are beginning to thrive. We can say with near certainty that none of this would be happening without the intervention of Vorasidenib. Furthermore, our son has only last week been informed that his MRI scans will, from now on, be every six months. This has further boosted his and our confidence in Vorasidenib and elevated our hopes for the future.
We fully appreciate that this medication is currently not a cure, but we know that it is effective and, furthermore, that there are emerging methods by which that effectiveness may be improved.
As a family, we have been daring to hope that Vorasidenib may soon begin to deliver a reduction in the size of our son’s tumour. We understand that our optimism is shared by many families in the brain tumour ‘community’.
“My son has returned to being more positive, chatty and so much more fun and happier. Almost the son I knew of pre 2019. He is planning a ski/ snowboarding trip for January which he has been reluctant to do for quite a while due to the seizures..
He has chosen ‘Watch & Wait’ twice now after second opinions from experts and I cannot contemplate how he would deal with the consequences of chemoradiotherapy and am not sure he would go through with this. He is determined to avoid therapy that might affect his cognitive function and his ability to work. Of course, therapy and time off work would also be a huge cost to the state.
We, his parents, are 77 early next year and the future for all of us, after the negative NICE decision, now feels again very bleak and uncertain.
I consider that it is too early with the curtailed trials to predict the long term positive effects of the drug. We read that it is so far showing reduction in seizures and even stopping the growth or reducing the tumour. It does seem to be doing this in my son’s case. We are bewildered that this possibility will be lost if unavailable to the small number of sufferers in England. Other family members and friends will be very sad if he has to return to the previous non Vorasidenib regime. He still works full time and travels abroad with a top trades events company; continues to live independently; socialises well and supports his friends and their families as well as ourselves. We are proud that he is independent and hasn’t claimed any state benefits so far.
These are some of the effects that this disease has had on my son and our family. Constant anxiety, uncertainty, lack of sleep, not being able to live a full life, stress, fractured family relationships, frustration of being unable to help him, happiness becoming rare or non existent and sadness. Life has not been the same for any of us involved since August 2019. His surgeon warned us!”
D
“As parents of a 27-year-old son diagnosed in mid-2024 with a low-grade oligodendroglioma (IDH mutant), we have lived through the extreme anxiety and uncertainty that accompanies the “watch and wait” approach. Our son is a police detective working on serious and complex cases — a job that demands sharp cognitive function, emotional resilience, and focus. Following his diagnosis and partial resection, we were told that further surgery, chemotherapy or radiotherapy would almost certainly result in lasting neurological and cognitive impairment, likely ending his career and dramatically reducing his quality of life.
During the initial watch and wait period, our whole family lived under a shadow of constant fear. Each MRI appointment brought weeks of mounting anxiety, sleeplessness, and intrusive thoughts about what the next scan might show. There was a pervasive sense of helplessness — knowing that a tumour was present but that no safe or effective treatment option was available. For our son and his wife, newly married and both in the early years of their careers, this uncertainty was devastating. For us as parents, it was heartbreaking to see their future clouded by fear rather than hope.
Everything changed when our son was granted early access to vorasidenib in January 2025. From that moment, the atmosphere within our family shifted from despair to cautious optimism. The knowledge that he was receiving a targeted treatment, supported by promising clinical trial results, gave him something profoundly important: hope — hope of delaying tumour progression, hope of avoiding the debilitating effects of radio- or chemotherapy, and hope of maintaining his ability to live a full and meaningful life.
The positive impact on his mental health has been striking. He has regained his confidence, his motivation, and his sense of purpose. The fog of anxiety that hung over him (and, by extension, us) has lifted to a great extent. He is once again able to concentrate fully on his demanding work and to plan ahead — something that had seemed impossible only months earlier. As parents, we have seen a visible and emotional transformation not only in him but also in his wife and siblings. There is a renewed sense of stability and normality in their lives.
C
“My son, age 29, was diagnosed with a grade 2 astrocytoma last year and underwent a craniotomy in February. He was accepted for Vorasidenib on the managed access programme. Had he not, there would have been no further treatment, just watch and wait – worrying for him and us. He so pleased to have this drug to delay regrowth of his tumour. It has given him hope that he will have longer to work and to enjoy his life. He is now really anxious that he will not be able to take the drug after the managed access program ends and that this may mean that his disease progresses more quickly, affecting his quality of life and ability to work”.
E
I am a 30 year old wife and a mum to 2 boys. We have a 4 year old and a 2 year old who we adopted a year and a half ago. I was diagnosed last August with a glioma which we later found out it was an astrocytoma. This diagnosis has radically changed my life I went from being a fit, healthy, independent mum to someone who needs to rely heavily on family support to get through every day.
Vorasidenib has helped me and given me hope in the midst of a very difficult time.
I had an awake craniotomy in November 2024 but they weren’t able to remove as much as they would have liked due to me having 2 seizures and a mini stroke during surgery.
As a result of the surgery I completely lost my ability to speak. I also started having more seizures, battled (and am still battling) cognitive fatigue, struggled with swallowing and weakness in my left leg and more. With the help of a number of professionals I have regained a lot of my abilities over the last year but I still have daily struggles with a number of things.
It has been a very slow recovery and has had a huge impact on our family and our wider family requiring a lot of support from them. But it has especially impacted the children. I couldn’t imagine the difficulty of going straight into radiotherapy and chemotherapy after the trauma of surgery and the effect that would have on our young family.
I regularly think about how I hope to see our children grow up, help our younger boy work through his adoption, find out what jobs they’ll have, watch them get married, and maybe even meet grandkids one day.
Every day I am on Vorasidenib is a day that I get without the long term effects that radiotherapy and chemotherapy have on the brain. It is another day to help me in my recovery from surgery. It is another day where I can hopefully my boys as they go through the milestones of life. And it is another day where I can give as much of myself as I can to my boys while they are so young.
For the sake of our young family and many others please approve Vorasidenib!
H
It is something that is close to my heart after being diagnosed with a Grade 2 Astrocytoma on 24th July 2025, at the age of 33, when my first baby was only 6 weeks old. I went into A&E on 13th July 2025 with persistent headaches, double vision and vomiting, was transferred to the John Radcliffe Hospital and had a craniotomy on 16th July, the day before my baby turned 5 weeks old. We returned home on 19th July.
I started Vorasidenib on 27th September via the Early Access scheme at Mount Vernon Cancer Centre and this has given me hope.
A
The current system offers almost nothing to someone in my position. Surgery is impossible without leaving me dead or severely disabled. Radiotherapy would destroy cognitive function and expose me to a lifelong risk of radiation induced malignancy. PCV chemotherapy, the only other option, carries severe toxicity. Roughly 1 in 50 patients die from treatment related secondary cancers such as leukaemia. The situation is so extreme that clinicians routinely delay treatment because the side effects of the available therapies are so damaging that allowing the tumour to grow untreated is considered safer than acting. This is the reality for patients with slow-growing but ultimately life-limiting brain tumours.
After my biopsy, I was placed on active surveillance. In practice this meant living with a progressing brain tumour and no treatment. The psychological burden is immense. Every day brings the same truth: the tumour continues to grow and there is nothing I can do. It corrodes mental health, destabilises families and removes any sense of agency.
By early 2025, my largest tumour began to grow more rapidly and developed a new enhancing focus consistent with aggressive transformation. I fought across three health boards to access Vorasidenib and eventually began treatment in July 2025. I am writing this on 4 November 2025, one day after receiving my latest MRI results. After three months on Vorasidenib, tumour growth has completely halted and the enhancing lesion has almost disappeared. I have experienced no side effects at all. For the first time since diagnosis, I have clear, objective evidence that treatment is working.
I currently access Vorasidenib in Scotland, only through the Royal Marsden compassionate use programme compassionate use programme. This support lasts for roughly 15 more months. Without SMC approval, my only remaining NHS options will be widespread brain irradiation or PCV chemotherapy. Both would permanently and severely compromise the quality of life that Vorasidenib has restored.
Brain cancer is the biggest cancer killer of people under forty. When young patients receive treatments that preserve cognition and normal life, we remain able to work, contribute to society, pay taxes and build our futures. When we are left with toxic or ineffective options, we lose decades of productive life to disability or decline. Vorasidenib allows me to continue studying, training, working and contributing as a fully functioning member of society. Removing access to it would reverse all of this progress.
Vorasidenib has not only stabilised my disease. It has given me back my life. I urge the SMC to approve it so that patients like me are no longer left with a choice between no treatment at all, or treatments so harmful that delaying them is considered medically safer than receiving them.
S
“Until someone has actually endured a life-changing experience, it is pretty much impossible to comprehend the impact of receiving a brain tumour diagnosis.
We live in Edinburgh and as the mother of a hugely capable (academically & physically) 22 year old boy, news of an inoperable and incurable brain tumour was both shocking and devastating. My life in these last 18 months has gone from one of quiet stability to one I don’t like and one I don’t recognise. I’ve always had an extremely close bond with my son but even more so, my feelings have become the mirror image of his. I feel his anxieties, his heightened stress, his frustrations and on dark days, his futilities. As a parent, I endeavour to cover these very real feelings up and present a positive front, in what can only be described as living nightmare – your life becomes a sham, masking your true dark thoughts.
Getting my now 24 year old onto Vorasidenib, when the only other options available were extensive chemo or radio therapies, has provided a real life line to navigate not just my son’s life to an adjusted normal, but that of my daughter, my husband and my own. Such a significant diagnosis at a prime stage of life (a life spent working hard at school and university combined with an elite athlete training regime) profoundly disrupted everything we as a family strove for, prompting unbearable conversations, while stealing hopes, expectations and ambitions for the future. The only thing that gives us hope is Vorasidenib.
Recent scan results after being on Vorasidenib have been massively encouraging – the concerning area of enhancement has shrunk – much to the relief and delight of us all.
In addition to the physical impact on the tumour, our family’s quality of life and mental well-being has certainly improved because Vorasidenib has allowed us to feel we are finally doing something to address the disease in a less catastrophic way than traditional therapies and certainly more than a watch and wait approach – I mean, Watch and Wait for What!!!!! There have been so little breakthroughs in the management of LGGs; it seems inconceivable that when one finally comes along (with encouraging results), we have to even consider it, let alone fight so hard for it. They say money can’t buy happiness – in this case it can certainly buy hope.
So while our son is on Vorasidenib through a named access program, managed between Scotland and London, we still remain anxious and concerned about what his and our future holds. However, we remain hopeful and that is what everyone needs in their life – without hope, what is the point?
My son asked his consultant oncologist “What would you do if your son was in my position?” I ask anyone involved in this process to ask themselves that same question
Vorasidenib is our hope – I implore you not to take our hope away”.
J
“I was deeply shocked and saddened when my nephew was diagnosed with a brain tumour in May 2024. The lengths my nephew and my brother and his family have gone to with respect to learning about the disease and possible treatments has astounded us all. After considerable effort and discussions with clinicians and MSP’s in Scotland we were relieved when he finally was able to get onto the Vorasidenib program. I cannot tell you what a positive impact this has had on everyone’s mental health. We are all rooting for him as I know he has so much to give. He has a proven track record of the ultimate in determination in both sporting and academic career to date and I believe that his determination in his professional field will lead to some amazing future chemical engineering breakthroughs – he must be given the chance to do this. He must be given the chance to live”.
F
“As a relative of a patient on Vorasidenib, I have first hand experience as to the true impact this innovative medicine has had on not just the immediate family but also the surrounding family too. We all live in Scotland and while the initial, out-of-the-blue LGG diagnosis was devastating (and always will be), it’s difficult to put into words just how much hope has returned to all our lives with recent encouraging scan results. Anxiety levels soar while waiting for results and the relief to hear the scan was stable after being on Vorasidenib has meant everything to everyone. Any cancer diagnosis is difficult, but for someone in their 20’s with so much to look forward to, having brain cancer is unbearably cruel. What is even more cruel is knowing there is a drug out there which has a proven track record (I have seen the scans) and there is a chance that it may not be available on the NHS – come on Scotland, please do not fail us”.
R
“I am the parent of a highly capable 24-year-old young man who was diagnosed with a low-grade oligodendroglioma. I hope to convey to the committee the profound importance of advances such as Vorasidenib in the modern treatment of brain cancers, particularly for young adults who have their entire lives ahead of them.
When my son was diagnosed, I witnessed the light go out of his eyes. The emotional and psychological toll of being told you have a brain tumour at such a young age is immense. The uncertainty, fear, and awareness of how current standard treatments can limit both lifespan and quality of life were overwhelming.
Vorasidenib has genuinely rekindled his hope. This is not naïve or false hope—it is grounded in his deep scientific understanding of how the drug works and how it fits into the evolving landscape of brain cancer treatment.
He has immersed himself in understanding IDH-mutant pathways, emerging targeted therapies, and future possibilities such as gene-based treatments. Vorasidenib represents, for him, the bridge that could carry him safely to further medical advances.
In his own words: “Vorasidenib is like catching the ultimate wave, which can carry me on to future treatments.”
Since diagnosis, my son has actively contributed to brain-related research here in Scotland, including investigating methods of delivering drugs across the blood–brain barrier using metal–organic frameworks. This demonstrates not only his determination to ‘keep going’ but also his commitment to contributing to scientific and medical progress for others.
Vorasidenib offers a vital alternative to aggressive treatments such as chemotherapy and radiotherapy, which come with significant long-term consequences, including:
• cognitive decline
• fatigue
• neurological damage
• reduced functional independence
• increased long-term healthcare needs
• diminished ability to work or study
In contrast, Vorasidenib provides disease control without the destructive impact of these treatments, allowing young adults like my son to maintain independence, productivity, and quality of life.
With access to Vorasidenib, patients like my son have a genuine chance to continue contributing to society through employment, research, and community involvement. Without it, they may face early disability, reduced economic participation, and significant care needs.
This medicine provides a window of stability that is both clinically meaningful and socially invaluable.
Vorasidenib is not simply another drug. For young adults with low-grade oligodendroglioma, it represents:
• hope grounded in science
- preservation of quality of life
- avoidance of harmful early treatments
- the possibility of living long enough to benefit from future therapie
- the chance to remain productive and independent
I respectfully ask the SMC to recognise the exceptional value of Vorasidenib and the life-changing impact it brings to the unfortunate few patients and families like ours”.
PATIENTS WHO HAVE HAD CHEMO AND/OR RADIOTHERAPY & FAMILY MEMBERS
B
“My wife has a grade 2 oligodendroglioma. She was on watch and wait for over 10 years before a year of radio and chemotherapy in 2019. Treatment was a very stressful year, provoking considerable anxiety and fatigue, and needing extensive travel and time off work for both of us across the year. Now back on watch and wait, it is an ongoing period of anxiety and impacts our quality of life significantly, with no further treatment available unless the tumour progresses”.
C
“I have a diffuse grade 2 astrocytoma and had surgery in May 2023. They were only able to remove 40% so I then had 6 weeks of daily radiotherapy followed by 12 months of chemotherapy. The treatments have left me with memory loss, lack of focus, reduced ability to retain information, poor attention span, increased seizures, increased infections, balance problems, nausea, IBS, anxiety and depression. The fatigue is relentless and I have been unable to return to my old job as a NHS trainee psychological practitioner”.
A
“So, I can’t have surgery, I can’t get hold of VORASIDENIB and my Oncologist is one of those who is giving it out on compassionate grounds, I’m not suitable for LITT and I’ve had my dose of R/T and am now living with the side effects of having no balance so my walking is shot so now use a walking stick and hold on to my husband, frequent falls, frequently forget what I was saying mid sentence and the list goes on”.
M
“I was diagnosed with an inoperable right parietal oligdendroglioma in 2018. My primary treatment was 6 rounds of PCV which controlled the tumour for 5 years. Last year a routine scan showed some minor growth so I had 30 radiotherapy sessions followed by adjuvant Temozolomide chemotherapy. Both types of chemo affected me badly(severe allergic reactions, constipation and fatigue) and had to be reduced. The radiotherapy has caused some improvement but I have a degree of short term memory loss and some slight visual deterioration since the RT. I currently suffer from bouts of fatigue, headaches and dizziness likely caused by the tumour. My mental health is ok, albeit with some mood swings”.
P
“As someone who has just completed chemo and radiotherapy I have experienced extreme fatigue at times alongside other side effects, not to mention the mental stress of the diagnosis and treatment.
No trials have been done as far as I am aware on patients who have had PCV chemo, but I think one is in progress for the drug in combination with TMZ (which isn’t the standard of care in the UK for my tumour which is a Grade 2 Oligodendroglioma)
Ruling patients out like myself is very frustrating as the drug does seem to delay progression in those who have it.
It does feel once again low grade patients get less research priority than those with higher grades which on some levels is obviously understandable, but we are no less important”.
P
“My daughter was diagnosed with a grade 2 Astrocytoma 3 years ago. Although much of it was removed she still needed radiotherapy and chemotherapy. This treatment left her unable to work for 2 years due to fatigue, learning to use her hand & arm again and learning to speak again. she is only recently started to build up her stamina. She is 39 and has a young child, all the family needed to help look after her, and her daughter. We are extremely worried as we have been told it will start to grow again, She has 3 monthly scans. What will happen when it does start to grow. I’m not sure she can go through the trauma and physical anguish of chemo & radiotherapy and I am now in my seventies and will not be able to care for her and my granddaughter easily. Vorasidenib is our only hope that it will stop the tumour growing and allow my daughter to look forward to a future where she will be able to continue working as a Vet and look after her 4 year old daughter”.
G
“My daughter has a grade II astrocytoma IDH mutant. She has had surgery, and this removed much of the tumour, and this was followed by radiotherapy and chemotherapy. However we are told it is likely to grow back, and that the only long-term solution is with Vorasidenib. After much effort with speech and physiotherapists, My daughter has now gone back to work. She pays her taxes”.
S
“We had no choice but to have our son undergo brain surgery that would last eight hours. He bravely accepted this, saying, ‘I am not brave; I have no choice’. He was and remains stoic. I am in awe of his resiliency and courage.
The weeks leading up to my son’s surgery made my stomach turn. I couldn’t believe my young boy would have to undergo a procedure to open his skull and remove a vicious tumour. To make matters worse, he was paralysed on one side for several weeks afterwards and had to learn to walk and use his right arm again, regaining full use only after many months. Four years later, he still feels that his right foot does not have the same dexterity it once had.
I was so proud and loved that he was born with the most perfect beautiful round head—. I know this sounds strange but I was. However, during his recovery, he developed a bone infection at the site where the skull had been opened, necessitating another surgery to remove the infected area. This left him with a literal large hole in the top of his head. We lived in constant fear of something falling on him or him bumping his head during this time. I was devastated; to me, it felt as if the surgery had disfigured him.
He eventually had a third surgery to place a prosthesis to replace the skull flap. I have two other children: one is autistic and has psychosis. The time my husband and I had to devote to our son impacted our ability to care for them both as well, which directly affected the well-being of our son with psychosis, leading to the threat of his mental health deteriorating further. If we had time and a respite period before further interventions we could have given more time (if we were not attending hospital appointments for chemo and radiotherapy)to our other children and our sons mental health may not of spiralled further.
One year and 3 surgeries later including a variety of cocktails of antibiotics later post-surgery. Sadly his 3 monthly routine scan only to discover that his tumour had started to I grow. We were advised to have intensive daily radiotherapy and six months of chemotherapy. At that time we had discussed the drug Vorasidenib but could not get access via any means or trials. We were devastated and my son’s worst fears of having to endure Radiotherapy and Chemotherapy were now the only option available unless you follow the tortuous cruel ‘watch and wait’ mantra to cast its devastation to strike its brutal invasion without warning. What a choice for a 22yr old young man who has already been through a year of experiencing continuous antiquated and barbaric treatments. He should have been making plans for his future not another year of being violently sick, scan after scan, blood tests, endless tireless hospital appointments and being further isolated and falling behind his peers and missing all the millstones every young wants to achieve in life. Losing any confidence he had and left with extreme anxiety. Another blow he would have to lose his driving license for even longer after radiotherapy. Due to our son’s high possibility of having further nocturnal tonic-clonic seizures we slept for more than a year on a mattress on his bedroom floor as we were so fearful after witnessing him unconscious several times previously and scared he would not recover and wake up. I regularly may hear a noise and get up to check my son is breathing.
I do not sleep at night worrying in case he has another life threatening seizure.
My husband had to take six weeks of unpaid leave to take him to the hospital every day during this challenging time so our income has been impacted. I have not been able to work now for many years due to my younger sons also have needs, and now there is little prospect of me being able to work again. We live very simple lives and rarely go out or take holidays we have not had a holiday for 7years. My son has a various gaps in his work history due to several years of treatment.
The radiotherapy and surgeries have left him with a large scar extending from above his ear to the upper left of his crown. He has been unable to regrow his hair after the radiotherapy.and chemotherapy his confidence is rock bottom and will not even answer the door without wearing a cap at all times in public. I can’t deny that his appearance has changed, and it saddens me that he has had to face this as a young man. We also notice that he is not as sharp mentally as he once was, and he tends to forget small things and gets tired very easily. He lost his independence as no longer able to drive relying on us for transportation. He has become
extremely nervous and riddled with anxiety. He tires easily more since his radiotherapy and chemotherapy and it affected his liver function.
We have had no release from worry and fear; the future brings more of the same without any let-up. Living day-to-day like this is incredibly challenging. If only he had been were allowed just a couple more for him to years to enjoy his life before brutal radiotherapy and chemotherapy. Also for a young man he missed on so many opportunities and the ability to build up more work experience, if he had his prospects now would be much better”.
